Introduction:
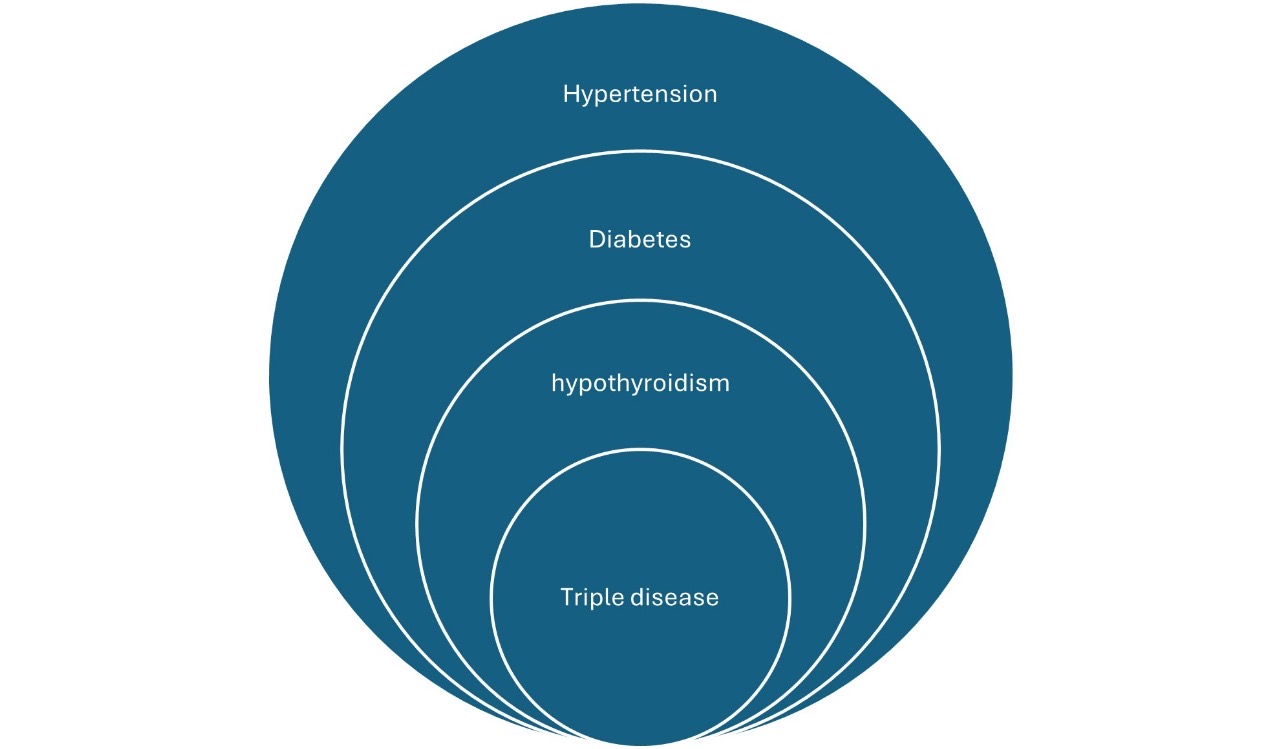
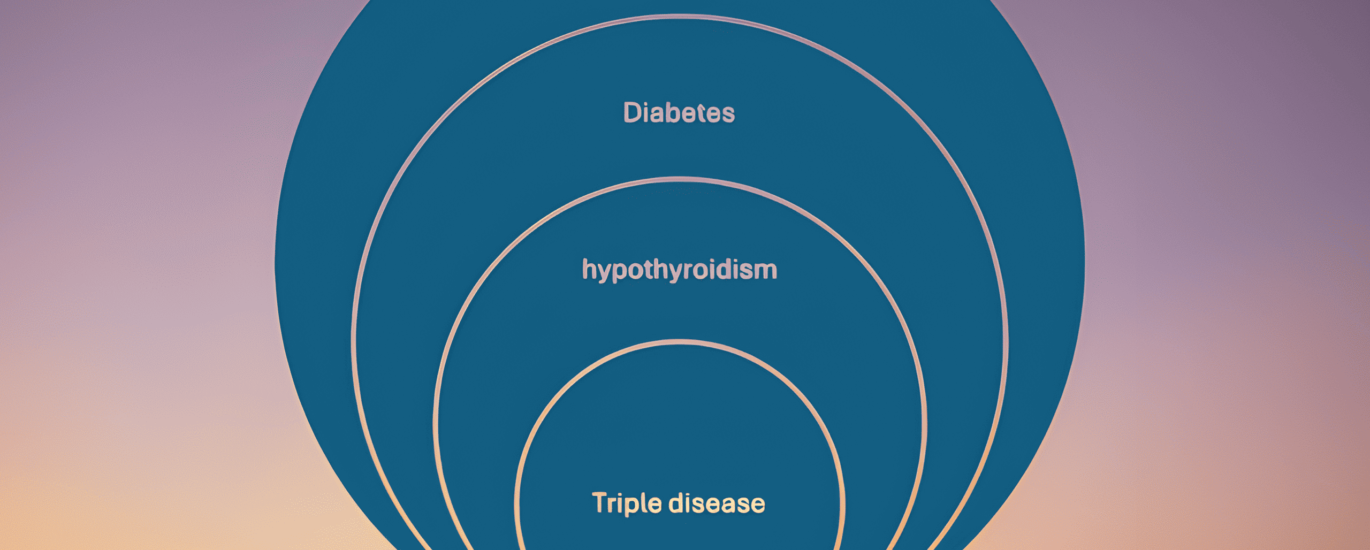
In modern clinical practice, the increasing prevalence of diabetes, hypertension, and hypothyroidism is becoming a significant public health concern. These conditions often co-exist due to common risk factors such as obesity, metabolic syndrome, and aging populations. Based on clinical observations, I propose the term “Triple Disease” to describe the co-occurrence of these three conditions. Additionally, I hypothesize that individuals with Triple Disease may have a higher likelihood of developing obstructive sleep apnea (OSA), a serious but often underdiagnosed condition.
Background:
• Diabetes and hypertension are well-known risk factors for cardiovascular complications. Similarly, hypothyroidism is associated with metabolic dysregulation and, in some cases, resistant hypertension.
• Current guidelines recommend screening for OSA in individuals with obesity, hypertension, and type 2 diabetes, but the connection with hypothyroidism is less explored.
• Sleep apnea has been shown to exacerbate insulin resistance, raise blood pressure, and negatively affect thyroid function, creating a vicious cycle of worsening comorbidities.Hypothesis:
I propose that the co-existence of diabetes, hypertension, and hypothyroidism, which I term “Triple Disease,” should prompt clinicians to screen for obstructive sleep apnea (OSA) in these patients. Although current diagnostic tools like the STOP-BANG questionnaire focus primarily on individual risk factors (e.g., BMI, snoring, age), Triple Disease may be a more comprehensive marker of underlying OSA.
Rationale:
1. Metabolic and Endocrine Interactions:
• Diabetes and hypothyroidism are both linked to insulin resistance and altered lipid metabolism. These shared pathophysiological pathways increase the risk of obstructive sleep apnea, which further exacerbates metabolic dysfunction.
• Patients with resistant hypertension, particularly those on three or more antihypertensive medications, have a higher prevalence of OSA.
2. Polypharmacy as a Red Flag:
• Polypharmacy (use of three or more medications) to control any one of these diseases should also be seen as a potential indicator of OSA. For example, patients requiring three or more medications to control blood pressure or glucose levels might have undiagnosed sleep apnea driving the need for aggressive pharmacological interventions.Clinical Implications:
Currently, these ideas are not widely accepted and are based on emerging clinical observations and pathophysiological understanding. However, if validated through randomized controlled trials and longitudinal studies, screening for OSA in patients with Triple Disease could:
• Improve diagnostic efficiency for OSA.
• Enhance the management of metabolic and cardiovascular conditions.
• Reduce the need for polypharmacy by addressing the underlying sleep disorder.Conclusion:
This hypothesis is proposed for further study and randomized clinical trials to validate the association between Triple Disease and OSA. Until more evidence is available, this concept remains an expert opinion based on clinical observation and the current understanding of the pathophysiology of these conditions.
Call for Research:
I encourage researchers and clinicians to explore this potential link through well-designed studies, as recognizing the connection between Triple Disease and OSA could lead to better integrated care and improved outcomes for patients with these chronic conditions.
Disclaimer:
Please note that this hypothesis is not yet supported by robust clinical evidence and remains speculative until further studies are conducted. It is intended to provoke thought and encourage investigation into this possible link.
to share your ideas- use comment button or visit our website.